Application of ionising radiation in healthcare
Application of ionising radiation in healthcare
Application of ionising radiation in healthcare is basic and routine in contemporary medicine. Benefits to patients from such application have been established beyond doubt (ICRP Publication 105 Radiological Protection in Medicine). It is difficult to imagine a healthcare system without modern diagnostic imaging and image-guided interventional procedures. A survey of policy leaders in internal medicine rated computed tomography (CT) imaging as one of the main healthcare innovations in the 20th century (Fuchs and Sox, 2001 [2]). The applications of ionising radiation in healthcare include the following topics.

Contents
Diagnostic Radiology
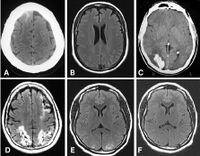
Diagnostic radiology, the imaging modalities using ionizing radiation, produces images of anatomical internal structures of human organs and physiological (functional) biological systems and helps significantly improve patient management and care in screening and diagnosis, assessing treatment response, predicting prognosis, and detecting disease recurrence. Modern diagnostic radiology assures faster, more precise diagnosis and enables monitoring of a large proportion of diseases. It has been estimated that in about one half of all cases, radiological procedures (conventional radiography, fluoroscopy, computed tomography) have a substantial impact on the speed of diagnosis and in a large fraction of cases they are of decisive importance in guiding patient management and therapy.
In diagnostic radiology, x rays, produced by machines, are transmitted through the patient’s body and detected by a receptor (or detection) system to generate the required image of the organs under investigation. The differential absorption of x rays in tissues and organs, owing to their atomic composition, is the basis for the various imaging methods used in diagnostic radiology. Modern diagnostic radiology uses a digital process for image acquisition, transfer, process and storage. Over the past years, with the tremendous technological progress and collaborative efforts in radiation protection, the radiation doses used in diagnostic radiology have been significantly reduced and continue to be reduced through technological innovations especially in CT (ICRP Publication 135 Diagnostic Reference Levels in Medical Imaging; ICRP Publication 121 Radiological Protection in Paediatric Diagnostic and Interventional Radiology; ICRP Publication 105 Radiological Protection in Medicine; ICRP Publication 93 Managing Patient Dose in Digital Radiology).
Diagnostic radiology are mainly applied in the areas: (1) Digital general radiology (DR); (2) Mammography; (3) Fluoroscopy systems; (4) Mobile radiography and fluoroscopy; (5) Bone density scan (DXA); (6) Computed tomography (CT); (7) Conventional tomography and tomosynthesis; (8) Dental radiography / CBCT; (9) Nuclear medicine including hybrid imaging (SPECT/CT, PET/CT, PET/MRI); (10) Cardiology; (11) Neuroradiology; and (12) Paediatrics.
Interventional Procedures
Interventional procedures using ionising radiation have revolutionised medicine in the past few decades for therapy and palliation, resulting in more patients being offered treatments that would not have been possible before with more invasive open surgery. The vast majority of interventional procedures are performed as “minimal invasive percutaneous therapies”.
As technology continues to advance, interventional procedures become more complex and some may take several hours to complete. New technologies with smaller catheters, guidewires, stents, filters and many other devices also present new challenges for radiological protection, such as aortic stent grafts, cardiac valve replacement, prostate embolisation, thrombus aspiration after stroke or selective internal radiation therapy (SIRT).
After CT, Interventional radiology is the second largest collective source of medical radiation exposure and, together with nuclear medicine the highest source of exposure to healthcare providers. ICRP has provided practical advice for physicians and other healthcare providers on the protection of patients and themselves involved in the interventions, for example in the following publications:
- ICRP Publication 139 Occupational Radiological Protection in Interventional Procedures
- ICRP Publication 121 Radiological Protection in Paediatric Diagnostic and Interventional Radiology
- ICRP Publication 120 Radiological Protection in Cardiology
- ICRP Publication 117 Radiological Protection in Fluoroscopically Guided Procedures outside the Imaging Department
- ICRP Publication 105 Radiological Protection in Medicine
- ICRP Publication 85 Avoidance of Radiation Injuries from Medical Interventional Procedures
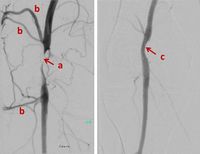
Physicians, assisted by nurses and radiographers, perform X-ray guided interventions as an alternative to conventional surgery. Most of these interventions are less invasive, the recovery periods are shorter, and for many types of interventions the complication rate is lower. In addition, some patients who may not tolerate anaesthesia and conventional surgery, as well as lesions that were not previously accessible, can now be treated by less-invasive image-guided interventions. In addition, interventional procedures offer new therapies where options of other medical specialties do not exist, such as embolization of liver tumours with chemical drugs or radioisotopes (SIRT).
The number of image guided interventions is increasing continuously in both developed and developing countries. New types of interventions are also of increased complexity, require extensive use of X-ray imaging, and raise new issues of occupational and patient protection.
Interventions are usually guided by fluoroscopy. Radiographic cine series or stored images from fluoroscopy are taken to document the outcome of diagnosis or treatment. Interventions can also be guided by computed tomography (CT) imaging, with images taken while the interventionalist steps behind a shield or out of the room, or by CT fluoroscopy, in which the interventionalist stays at the patient for obtaining images during device manipulation.
Radiation Therapy
Radiation therapy utilizes ionizing radiation to treat malignant and benign diseases. It has become a standard of care for treating many types of cancer. Current medical practice uses radiation therapy in about half of all newly diagnosed cancer cases. Radiation therapy works by exploiting radiobiological differences between cancer and normal cells/tissues, and by depositing radiation dose in cancer tumours while keeping doses to surrounding normal tissues below damaging thresholds as much as possible.
Radiation therapy is used as a primary, curative treatment, as a palliative treatment, and/or as adjunctive therapy. It can be used pre-operatively or post-operatively, and in combination with chemotherapy, biologic agents, and hormonal agents. The radiation dose prescribed to achieve tumour control is often limited by the radiosensitivity of normal tissues, which are located around the tumour, and thus may result in early and late adverse side effects. Some adverse effects are unavoidable and often resolve spontaneously or with treatment. Serious adverse effects may occur and result from the proximity of sensitive normal tissues to the treatment area. However, such adverse side effects do not undermine the purpose of radiation therapy. Appropriate use of radiation therapy saves millions of lives every year. Even if only palliative treatment is possible, the therapy reduces suffering substantially. There are also a few non-malignant diseases whose treatment by radiation is a method of choice. Note that palliative radiotherapy and radiotherapy of non-malignant diseases uses much lower doses, generally not inducing any acute side effects.
Radiation therapy has benefited greatly from technological advances over the past two decades, resulting in a wide variety of available delivery methods: Intensity-modulated radiation therapy (IMRT) utilizing techniques to quantify the critical normal tissue doses; Image-guided radiotherapy (IGRT) utilizing real-time imaging for treatment localization during radiotherapy; Stereotactic radiosurgery (SRS) delivering of a large dose per fraction to treat focal brain lesions and its extension, stereotactic body radiation therapy (SBRT), to treat focal lesions in the lung, spine, liver, pancreas, prostate and all parts of the body; Particle beam radiotherapy utilizing protons, neutrons or other heavy particles; Brachytherapy placing sealed radioactive sources near the tumor; Intraoperative radiotherapy (IORT) delivering to the surgical bed after removal of the tumor or to the tumor itself at the time of surgery; Unsealed sources delivering a radiopharmaceutical orally or parenterally; and Hyperthermia adding of heat to radiotherapy.
The advance of technology inevitably results in an increase in complexity and opportunities for new types of human error and equipment problems. Ongoing education and training of members of the radiotherapy team with respect to new and evolving technologies is crucial, as is adherence to clearly defined quality assurance policies and procedures.
- ICRP Publication 112 Preventing Accidental Exposures from New External Beam Radiation Therapy Technologies provides recommendation and guidance on preventing accidental exposures from new external beam radiation therapy technologies
- ICRP Publication 97 Prevention of High-dose-rate Brachytherapy Accidents and ICRP Publication 98 Radiation Safety Aspects of Brachytherapy for Prostate Cancer using Permanently Implanted Sources discuss safety aspects of brachytherapy
- ICRP Publication 127 Radiological Protection in Ion Beam Radiotherap addresses protection in ion beam radiotherapy
- ICRP Publication 86 Prevention of Accidents to Patients Undergoing Radiation Therapy covers prevention of accidental exposures to patients undergoing radiation therapy
Nuclear Medicine
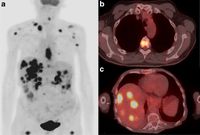
Nuclear medicine uses radioactive substances, called radiopharmaceuticals, in the diagnosis and treatment of a range of diseases. These substances are chosen or especially developed to be taken up predominantly by one organ or one type of cell in the body. Nuclear medicine offers unique diagnostic information in oncology, cardiology, endocrinology, neurology, nephrology, urology and other areas. Such information is not obtainable, or obtainable only with less accuracy, by other modalities. For nuclear medicine diagnostic procedures, trace amounts of radiopharmaceuticals are administered to patients through injection into veins (intravenous), skin (intradermal) or tissues (intraparenchymal) as well as breathing in (inhalation) or eating/drinking (ingestion). After intake, the function, or physiology, of various tissues, organs or organ systems can be demonstrated. For example, in cancer patients, nuclear medicine imaging can be used for diagnosis (i.e. is a cancer present), staging (i.e. how far has it spread), assessment of response to therapy or of possible disease recurrence. Nuclear medicine cameras are now commonly combined with a CT unit (e.g. hybrid SPECT/CT and PET/CT) which allows precise anatomic localisation of pathology. (Figure 8, Figure 6, 7)
Nuclear medicine procedures for treatment are non-invasive and present no risk of direct complications to patients, but limited to several well-established situations where killing hyperfunctioning or malignant cells is important (for example hyperthyroidism, cancer of the thyroid, degenerative and inflammatory diseases of joints, palliative treatment of metastases to the skeleton). In addition, there are many studies showing significant potential for radio-labelled antibodies and receptor-avid peptides to be used in the treatment of several malignancies.
A patient undergoing nuclear medicine imaging or treatment becomes a radiation source and remains “radioactive” after the radiopharmaceutical has been administered. Radiation protection advice depends on the specific radioisotope and its radiopharmaceutical form administered and whether the procedure is diagnostic or therapeutic. However, the general principles of the ICRP system of radiological protection apply in nuclear medicine as they do for other medical imaging modalities using ionising radiation. In addition ICRP Publication 52 Protection of the Patient in Nuclear Medicine (and Statement from the 1987 Como Meeting of ICRP) and ICRP Publication 94 Release of Patients after Therapy with Unsealed Radionuclides provide recommendations and guidance on the protection and release of patients after therapy with unsealed radionuclides (e.g. post 131 Iodine therapy for thyroid cancer), and ICRP Publication 128 Radiation Dose to Patients from Radiopharmaceuticals: A Compendium of Current Information Related to Frequently Used Substances provides dose coefficients to patients from radiopharmaceuticals.
Biomedical Research
Ionising radiation is widely used in biomedical research. Such research is normally carried out in the laboratory and using different animal models. Research on normal tissue radiobiology aims at the investigation of the pathophysiological mechanisms and the consequences of ionising radiation. Pre-clinical in vivo studies in experimental animals largely focus on the characterisation of the pathophysiology of normal tissue reactions, the identification of potential biomarkers or the establishment of assays for predicting normal tissue toxicity of radiotherapy. Establishment of tumor xenograft models, involving implantation of human patient-derived tumors into immunodeficient animals, is a valuable research tool to investigate the biological effects of ionizing radiation on the disease mechanism of cancer.
Studies involving radiation exposure of patients adds another level of risk that must be evaluated by an institutional ethics review board with assistance of a radiation expert or radiation safety committee. In all investigations involving exposure of humans, a careful estimation of the radiation dose to the patients or volunteers should be made. The associated risks should then be weighted against the benefits for the patients or the society when volunteers are involved. A reasonable alternative is the ex-vivo exposure of tumor specimen, human blood or skin samples obtained from patients or healthy volunteers, to avoid the hazard of radiation exposure. Approval by an institutional ethics review board or human studies committee must be obtained prior to conducting human subject research. The researchers' role is to conduct their research ethically while maximizing benefits to the society and minimizing harm to the participants. ICRP has provided recommendations in the guidance ICRP Publication 105 Radiological Protection in Medicine and a previous ICRP Publication 62 Radiological Protection in Biomedical Research.
Veterinary Medicine
Just as in human medicine, the use of ionising radiation in veterinary care serves to provide or assist in providing a diagnosis, to guide an interventional procedure or to provide a direct radiation-induced therapeutic benefit. The use of diagnostic radiology is widespread in veterinary care, in veterinary clinics or in private practices. Smaller companion animals are typically radiographed at the practice or clinic, whereas larger animals may also be radiographed at farms, zoos, or at riding and selling stables. Film-screen radiography is being replaced more and more by digital imaging techniques; CT and CBCT scanning have become routinely available in larger animal clinics. Fluoroscopically guided interventional procedures are also used in veterinary medicine. In these procedures, the radiation serves to provide dynamic, real-time images. The images will guide the anatomically correct delivery of treatments and will often allow real-time visualization of the results of the intervention.
Nuclear medicine techniques are used in veterinary care as well. Diagnostic nuclear medicine procedures provide more information on the functioning of organs and tissues than radiographies, but the morphological information provided is less detailed. For these reasons, diagnostic nuclear medicine is more and more being combined with CT-scanning. Such examinations are referred to as “mixed modality” or “hybrid imaging”, with SPECT-CT and PET-CT as typical representatives. A more recently developed combination of nuclear medicine with magnetic resonance imaging (MRI) is also possible and provides similar advantages.
In therapeutic nuclear medicine procedures a much higher dose (“activity”) of radioactive substances is administered to the animal. The radiation dose delivered to the targeted tissue or organ then becomes so high that cells within this tissue or organ are inhibited in their proliferation or even eliminated. If a cancer is being targeted, complete elimination of the cancerous growth is the desired objective. But in treating other diseases such as hyper functioning of the thyroid gland or inflammation of the joints, inhibition or partial destruction may be sufficient for achieving the desired clinical goal. In the more classical radiotherapy, radiation generated outside the animal patient is also used to eliminate tissues that are undesired. Most often this will be used for treating animal patients affected by cancer.
ICRP has recently established a task group (TG110) to develop recommendations on the protection of veterinary patients, veterinarians and their co-workers, animal owners and handlers providing care to the patients or comforting them. Radiation exposures to the veterinarians and their co-workers, as well as owners and handlers of the animal can be very different. Radiation dose resulting from a single examination is typically very low, but veterinarians and their co-workers performing multiple examinations may receive non-negligible dose. Some applications that are newer in veterinary medicine, such as CT-scanning, interventional radiology procedures, nuclear medicine diagnostic procedures and radiotherapy procedures, have the potential to cause much higher exposures and should therefore be performed with explicit attention to radiation protection. In the case of nuclear medicine procedures and the use of small implantable radioactive sources for radiotherapy purposes, radioactive substances and objects may be spread outside of the veterinary clinics and thus become an additional risk factor in the human environment.
More In-Depth Information
If you are looking for something more extensive look no further below are a collection of related links and articles that can provide more information on this topic!
Diagnostic Radiology
| International Atomic Energy Agency - Radiation Protection of Patients (RPOP) | https://www.iaea.org/resources/rpop |
| Radiology Information Resource for Patients | https://www.radiologyinfo.org |
Radiation Therapy
| American Society for Radiation Oncology | https://www.Astro.org |
| European Society for Radiotherapy and Oncology | https://www.estro.org |
| International Atomic Energy Agency | https://www.iaea.org/resources/rpop |
References
Radiation Therapy
Yoon, H., Shah, K., Small, W. Jr., Mehta, M., Hayes, J., Chapter 1: Basic Concepts of Clinical Radiation Oncology. In: Clinical Radiation Oncology, 3e. Small, W. Jr., (ed): John Wiley & Sons, 2017, pp. 3-14.